After the FDA approved the Dexcom G5 Mobile CGM for use in treatment decisions, the Endocrine Society convened expert panels to address questions about how patients should use the trend arrow information when fine-tuning their insulin doses. The new approaches ensure that both adult and pediatric patients will have a “practical approach” to using the trend arrows to adjust insulin doses.
Continuous glucose monitors (CGMs) have had a great impact on improving diabetes care, and their influence will only grow with recent government approvals expanding their use.
Late last year, the U.S. Food and Drug Administration (FDA) approved the Dexcom G5 Mobile CGM System (Dexcom G5) for patients with diabetes to make insulin dose decisions without needing confirmatory fingerstick testing. This is the first CGM to receive such an FDA approval. And early this year Medicare announced it would begin covering the devices for qualified patients.
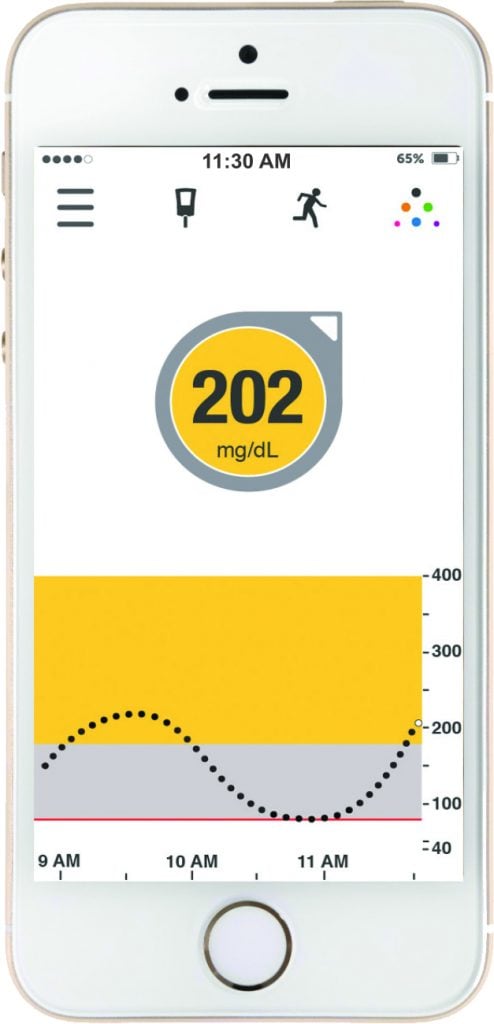
CGMs continuously measure interstitial glucose as frequently as every five minutes to give patients much more insight into their changing glucose than traditional blood glucose monitors. Certain devices, such as the Dexcom G5 Mobile CGM system (Dexcom G5), transmit that data in real-time to give patients alerts and alarms for low or high glucose levels are and even how fast glucose is changing.
The rate that glucose is changing is shown as a “trend arrow.” Trend arrows give patients and the people caring for them a tremendous amount of information in a single set of symbols. These arrows show how fast glucose is changing – up or down. This can be a powerful tool to plan ahead, prevent dangerous low or high glucose levels, and adjust the amount of insulin you might take.
In the case of the Dexcom G5, all that data can be sent to a pocket-sized receiver, compatible Smart device, or even shared through an app with loved ones or doctors. But how are trend arrows being used? If the arrows are going up, you might take more insulin. If they’re going down, you might take less. But how much more or less? There are a couple methods available, but they have drawbacks in how they are used across pediatric and adult patients.
The Endocrine Society has taken a leadership role to ensure the safe and effective use of the Dexcom G5 trend arrows when adjusting insulin doses with a pair of publications by expert panels that developed a “practical approach” for children and adults.
- The FDA has recognized advances in continuous glucose monitoring technology by approving the Dexcom G5 CGM System to be used for treatment decisions including insulin dosing in patients with diabetes.
- The Endocrine Society responded to the FDA decision by convening two expert panels to develop approached for how patients can use “trend arrow” information to adjust insulin dose decisions.
- The expert panels created simplified approaches that can be widely and safely used by patients to fine-tune their insulin doses.
- Future discussions are needed on how this approach could be used in other CGM systems and special patient cases.
Endocrine Society Advocacy
In its clinical practice guideline on diabetes technology issued in September 2016, the Endocrine Society recommended CGMs as the gold standard of care in type 1 diabetes, and the Society has been advocating for FDA approval of this expanded use in insulin dose decisions for some time. “The Endocrine Society believes that CGM is lifesaving technology that is yet another tool to help people with diabetes effectively manage their disease,” Nicholas Argento, MD, diabetes technology director at Maryland Endocrine and Diabetes in Columbia, Md., testified to the FDA Clinical Chemistry and Clinical Toxicology Devices Panel in July 2016.
“The Dexcom CGM has been proven to be accurate enough to allow direct treatment,” he said, pointing out that patients are already using it for insulin dose decisions, but had no guidance on how to do so. Official FDA recognition of this de facto use would improve patient safety by freeing the manufacturer and others to develop recommendations on how best to use the CGM data.
“These perspectives serve as a starting point,” Laffel adds. “In the current era of increased penetration of advanced of diabetes technologies in routine care, we will be able to further refine these recommendations when more empiric evidence becomes available.” – Lori Laffel, MD, MPH, chief of the pediatric, adolescent, and young adult section, Joslin Diabetes Center; professor of pediatrics, Harvard Medical School, Boston
During the approval process, FDA officials noted their agreement with this position and the need for information for physicians and patients. Once the FDA issued its approval, the Endocrine Society convened two expert panels to develop and publish approaches to using the trend arrow information; one for adult patients and one for pediatric patients. The panels aimed to have their publications ready by November, Diabetes Awareness Month. The approaches to using trend arrows will be published in the Journal of the Endocrine Society by the end of the year.
Embracing Advanced Diabetes Technology
“We have had various CGM devices available for almost 20 years. Since the early generation devices, and there have been tremendous improvements in device performance,” says Lori Laffel, MD, MPH, chief of the pediatric, adolescent, and young adult section at the Joslin Diabetes Center and professor of pediatrics at Harvard Medical School, who chaired the pediatrics expert panel. “[Dexcom G5] can provide up to 288 glucose readings each day and are approved for up to seven days of consecutive wear. The diabetes community, including providers and patients, embraces this advanced technology that has demonstrated improved performance and usability. CGM helps patients to improve their glycemic control without increasing their risk for hypoglycemia. Clinicians and patients along with family members now need tools to use these devices effectively and safely. Our expert panels wanted to create a usable, easy-to-implement approach to fine-tune insulin doses using the CGM data and trend arrows. We all wanted to create a method that could be readily taught and implemented in the diverse population of pediatric and adult patients with insulin-treated diabetes.”

Starting an Important Conversation
The new approach is based on “previously published algorithms…, clinical experience as endocrinologists, and guidance from other diabetes specialists,” the pediatric document says. “Although there is a wealth of clinical experience, we don’t have clinical trials that have actually verified the various algorithms we reviewed, so this publication would not fall in the category of a true guideline. Rather, this is a perspective paper with a practical approach for the CGM users and their healthcare providers,” Aleppo says.
The approaches from the expert panels are a starting point for a much needed discussion in the medical community on how to best use trend arrow information in the Dexcom G5 as well as across other CGM devices as indications for using in insulin dose decisions expand. There will also be opportunities to put these approaches into clinical studies and discuss how they could be used in special patient circumstances.
A Practical Approach
The expert panels developed approaches that take into account the patient’s established correction factor (also called insulin sensitivity). For each range of correction factors, the authors suggest an insulin dose adjustment that is given as an increase or decrease in insulin dose depending on the direction of the trend arrow(s). The approaches also take the wide range of correction factors in adult and children patients into consideration as well as the limitations of patient’s using insulin pens that can only deliver insulin in 1.0 or 0.5 unit increments. The end result is an approach that is safe and easy to use for a wide range of patients on different treatment plans.
Importantly, the adjustments aren’t a substitute for typical calculations. The perspectives note that “adjusting insulin doses using trend arrows does not replace standard calculations. [It] is an additional step that increases or decreases the insulin dose that has been calculated using standard parameters.” Laffel calls this “fine-tuning” the insulin dose.
The Dexcom G5 indicates the rate of change by displaying trend arrows: two arrows pointing straight up or down mean rapidly rising or falling glucose; a single arrow pointing up or down denotes rising or falling glucose; a single diagonal arrow pointing upward or downward means slowly rising or falling glucose; and a horizontal arrow represents a steady glucose level.
The heart of each approach is a table of suggested insulin dose adjustments based on the direction of the arrow(s) and the patient’s correction factor. For example, a single rising arrow indicates:
- for an adult patient who has a correction factor less than 25, an insulin dose adjustment of +3.5 units;
- for an adult patient with a correction factor of 25 to <50, an insulin dose adjustment of +2.5 units;
- for an adult patient with a correction factor of 50 to <75, an insulin dose adjustment of +1.5 units; and
- for an adult patient with a correction factor of 75 or more, an insulin dose adjustment of +1.0 unit.
Differences for Adults and Children
For both adults and children, the panels suggest that patients start adjusting insulin doses conservatively until they gain experience. But the panels also call out the differences in how to approach adjusting insulin doses in adults and children.
In the adult approach, the panel suggests special guidance for up to 4 hours following a meal that reduces the risk low and high glucose levels and prevents insulin “stacking”. This is because meals can have variable effects on glucose that impact trend arrows and adults tend to eat less frequently than children and want to correct soon after eating. For these reasons, the adult paper has a special table for postprandial monitoring and treatment. The paper also highlights the caveats in using the approach in frail and elderly individuals.
“Medicare patients with diabetes are now able to use CGM technology, which will keep them safer. They will feel empowered when they see that the interventions they make result in a huge difference for their glucose control.” – Grazia Aleppo, MD, associate professor of medicine; director, Diabetes Education Program, Northwestern University, Chicago, Ill.
The pediatric guidance notes that treatment is complicated by the fact that insulin sensitivity changes with age, and divides patients into three broad categories of pre-school-age/toddlerhood (ages two to six), school-age/middle childhood (ages seven to 12), and adolescence/young adulthood (ages 13 to 22). “Insulin sensitivity is generally greater in younger, pre-pubertal patients and decreases over time as youth age with decreasing insulin sensitivity associated with pubertal growth and development,” it notes. In young adults who have completed pubertal growth and development associated with adolescence, insulin sensitivity often increases again, Laffel says.
But age is just one factor that these papers consider in trying to provide “custom-tailored treatment,” Aleppo says. “I tell my patients who use CGM in non-adjunctive fashion that they always need to consider where they are in the moment: are they sick, did they just eat, are they exercising, did they take acetaminophen? When people with diabetes engage in aerobic exercise, even though they might see one arrow trending up on their CGM, may be more insulin sensitive from the exercise, therefore they should use caution and not be as aggressive in taking a correction compared to other circumstances.” Each document contains sections addressing these kinds of variables.
- Seaborg is a freelance writer based in Charlottesville, Va. He wrote about bioidentical hormones in the October issue.
Four reasons the Endocrine Society supported approval of the use of CGM for treatment decisions:
* “Dexcom CGM has been proven to be accurate enough to allow direct treatment…and enables patients to make safe and timely treatment decisions.”
* “Patients are already making real-time treatment decisions based on their CGM data without fingerstick verification, and doing it effectively and safely.”
* “Doing proper and accurate fingerstick verification is often highly impractical if not impossible in the workplace and doing so could put others in danger of exposure to blood products.”
* “Patients need guidance on using unverified CGM data safely and effectively. FDA’s approval of this change would enable Dexcom to offer patient support and education on the best ways to use unverified CGM data in real time.”
From the testimony of Nicholas Argento, MD, on behalf of the Endocrine Society to the FDA Clinical Chemistry and Clinical Toxicology Devices Panel on July 21, 2016.


