An Endocrine Society member since 1979, John William Honour, PhD, FRCPath, used his time in lockdown to write a voluminous tome on steroids. He talks to Endocrine News about his recent book, Steroids in the Laboratory and Clinical Practice, how it was impacted by the COVID-19 pandemic, and why it may just be the definitive book for endocrine researchers and clinicians alike.
Last year, John William Honour, PhD, FRCPath, a retired consultant clinical scientist at University College London Hospitals in the U.K. with more than 45 years of laboratory work in steroid endocrinology, published Steroids in the Laboratory and Clinical Practice, a comprehensive reference book that addresses the specificity of steroid determinations which can clarify confusion clinicians face with abnormal laboratory results.
Published by Elsevier, Steroids in the Laboratory and Clinical Practice includes all the information needed to understand the key concepts in of steroid synthesis, action, and biological effects. When faced with a patient and a steroid-related problem the biological tests, their results, the alternatives, reference ranges, and algorithms leading to a diagnosis of a disorder of the system need to be understood. This is a complex and fast-changing field with many unanswered questions with opportunities open to create future challenges. The book covers both basic and analytical applications of steroids to medicine in one source.
Endocrine News spoke with Honour to talk about his career, how the COVID-19 pandemic impacted his writing process, and why this book should be the “go-to” book for clinicians, researchers, pathologists, laboratorians, analytical biochemists, and students interested in this group of hormones that has fascinated him for half a century.
Endocrine News: What attracted you to biochemistry? From there, what led you to endocrinology and the study of steroids?
John William Honour: I came to biochemistry from work experience in a bacteriology laboratory. Organisms were cultured on petri dishes covered with a layer of agar. If bacteria were present they multiplied and formed colonies. From there some of the bacteria could be transferred to a microscope slide and stained with dyes before viewing under the microscope. The bacteria are seen as cocci, rods, spiral and other shapes. Organisms were also put into sugar solutions to see if they produced gas or a change in colour of the solution to indicate formation of acids. I wanted to know about the reactions that caused these changes which is why I wanted to study biochemistry.
I received a Bachelors degree in Applied Biochemistry from Bath University in 1972 where I conducted my first research in steroids (with Professor R Hardisty) by studying changes in enzyme activity of testes of Lampreys as they migrated from salt to fresh water to reproduce and die. After graduation I started my professional life as a Senior Research Officer at the MRC Clinical Research Centre (CRC) in Harrow, England that was based on the NIH, Bethesda model. I completed a PhD in Biochemistry from the University of London in 1978 supervised by Cedric Shackleton and Professor Vivian James. My education in the application of mass spectrometry (MS) for steroids was due to Cedric who has continued to pioneer studies using MS technology. I have from the outset used steroid profiling to look at multiple steroids in one analysis, this is now often referred to as metabolomics.
Gas chromatography – mass spectrometry (GC-MS) was in 1972 really new, yet remains a powerful analytical tool for steroids with better resolution than high pressure liquid chromatography (LC). The success of LC with MS came when spray techniques at the interface with a mass spectrometer enabled coupling of the two elements. LC-MS does not require derivative formation thus saving valuable time in a hospital laboratory processing hundreds of samples each day.
EN: What have been some of the most rewarding – and most challenging – moments from your career?
JWH: The PhD thesis was titled ” Application of gas chromatography and mass spectrometry to the investigation of human mineralocorticosteroid metabolism”. I worked with clinicians to study patients with adrenal problems, mainly young children. Demonstrating the role of aldosterone in salt loss of preterm infants gave rise to my first steroid publication. I also collaborated at Great Ormond St Hospital (GOSH) for children in studying patients with salt loss, disorders of sexual development, hypertension and growth.
An eureka moment came from the results of analysis of urine steroids of a patient with 17-hydroxylase deficiency who did not produce cortisol because the enzyme to convert corticosterone to cortisol was defective. I demonstrated an enterohepatic circulation of corticosterone and bacterial metabolism of steroids in the intestine, as previously described in rats with corticosterone as the principal glucocorticoid. Some steroid reactions such as 21-dehydroxlation had earlier been shown by Jan Sjovall, Hakan Eriksson, Jan-Ake Gustafsson and colleagues at the Karolinska Institute to be absent in germ-free rats. I was awarded a Postdoctoral Fellowship of the American Heart Foundation with Edward Biglieri at University of California, San Francisco to explore further there in 1978-1979 the role of bacterial steroid metabolism in the intestine which set my track to continue this line of research.
I was able to conduct experiments on returning to the CRC that showed experimental hypertension in Wistar and stoke-prone rats could be prevented by treatment with antibiotics. This was probably the first time that bacterial steroid metabolism was linked to hypertension, predating claims made in 2015 when a new term, the microbiome, was popularised.
I was fortunate to be married to Pauline who was a bacteriologist with a veterinary background that was valuable to her when she was the first to see the anaerobe, Clostridium Difficile, in biological samples from patients with Irritable bowel syndrome. We tried at that time to characterise the intestinal flora of the rats I was studying. It was laborious and inconclusive, most of the organisms being anaerobic and acutely sensitive to air. That work would have taken a different journey if 16S RNA sequencing in use today had been available then. At that time bacteriology was limited to the tests I already described. Thirty years later the gut microbiome is acknowledged to contribute to many pathological processes. The number of bacteria in the gut are realised to exceed the number of cells in the human body and much research on the impact of the microbiome on homeostasis and pathology will follow.
EN: Tell us about your involvement with the Endocrine Society. What or who got you involved with the Society? Are there any special moments, say at ENDO, that you can reflect on?
JWH: I joined the Endocrine Society in 1979 and have regularly attended ENDO. I travelled widely to scientific conferences across Europe, USA and Australia with regular attendance at ENDO. This afforded the opportunity for networking with other steroid research “stars” and “up-coming stars”, which provided important opportunities to recognise new research elements and exchange results and ideas. I count many heroes in the Society – Cedric Shackleton, Walter Miller, Maria New, Bert O’Malley, John Funder, John Coglan, Perrin White and emigrants from UK – Evan Simpson, Robert Carey, David Morris and others. In UK I have high regard for my colleagues at UCL also Sir Christopher Edwards, Paul Stewart, Stafford Lightman and others. I am now an Emeritus member of the Society. I particularly remember a satellite meeting to the 9th International Congress on Hormonal steroids 21-23 September, 1994 in Lake Murray Resort, Ardmore Oklahoma when Doug Stocco and Barbara Clark reported the discovery of StAR – the steroidogenic acute regulatory protein that was involved with the transport of cholesterol into the mitochondria – the first step in the biosynthesis of the steroid hormones.
EN: Now to your book. Can you give us an overview of Steroids in the Laboratory and Clinical Practice and what readers could expect from it?
JWH: The book covers in three parts: basic chemistry, methods for steroid analysis, and clinical application of steroids in a single source. The comprehensive reference book addresses the specificity of steroid determinations to clarify confusion arising from the laboratory results. The book covers important advancements in the field and is a valuable addition in the literature addressing all existing knowledge gaps. I hope the book will be a “must have” reference for pathologists, laboratorians, endocrinologists, analytical/clinical chemists and biochemists. The book is particularly useful in three areas:
- Addresses the normal production of steroids and concentrations found in biological fluids and tissues
- Presents the changes in steroid concentrations at life events as reference points for clinical investigations
- Reviews the genetic disorders of steroids in relation to specific enzyme changes and clinical presentation
Puberty, pregnancy and menopause are obvious life events but there are others known to endocrinologists such as a phenomenon of mini-puberty in the months after birth due to an activation of the hypothalamic-pituitary-gonadal axis that is then suppressed until puberty. Adrenarche is a period at five to nine years of age when a new reticularis zone develops in the adrenal cortex and remains active until senior years when the important secreted steroid dehydroepiandosterone sulphate (DHAS) declines. These changes need to be considered particularly in the investigation of patients with infertility, sex development disorders and gender dysphoria.
The book is somewhat a summary of my broad experience of steroid endocrinology over 45 years. No such book had been published since “Steroid Hormones” by David Gower in 1979, but much has changed since then.
EN: You write about the need for early biochemical assessment as key to providing adequate clinical diagnosis and preventing life-threatening adrenal crises. Can you speak a little more to that?
JWH: On ward rounds I saw the sick children with adrenal disease and encountered the parents of children who could not answer the question everyone asked them, “Is it a boy or a girl?”. I learned the laboratory needed to act promptly on any investigations of these patients. Clinicians struggled with the chemistry of steroids despite what seems to me a structure of four rings. To clinicians a group of steroids when drawn out looks like chicken wire.
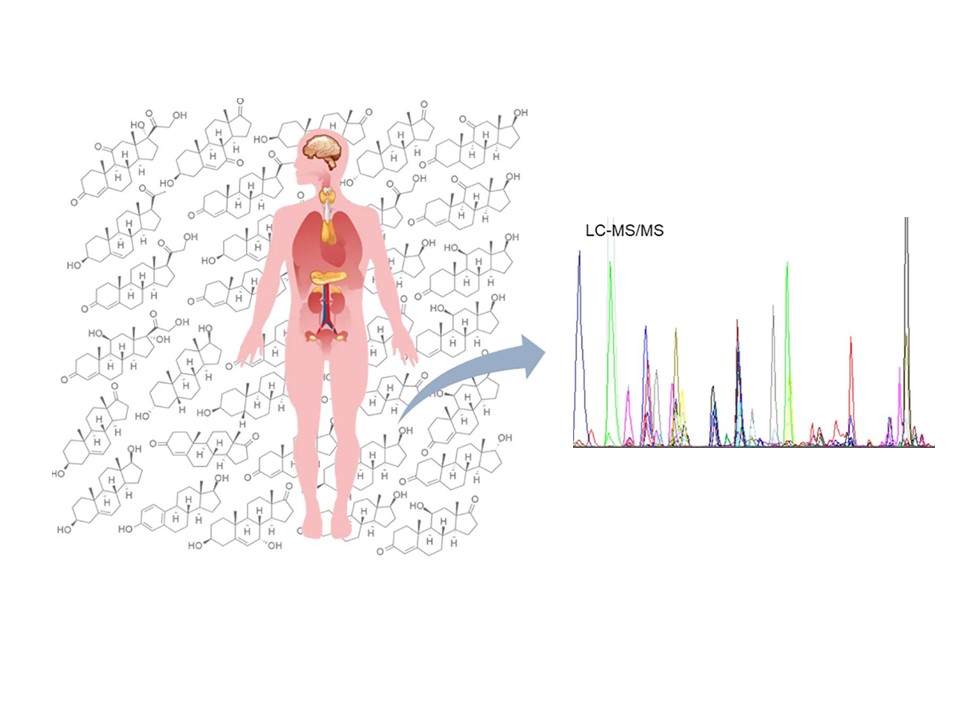
These days multiple steroid analysis is becoming more feasible for diagnostic testing because LC-MS/MS can be programmed for targeted analysis of tens of steroids provided that steroids of the same molecular weight are separated in the chromatograph. I have found it necessary to take a gentle approach to help the reader of the book and lecture audiences to get to understand steroid chemistry.
In 1983 I accepted a Senior Lecturer position at the Middlesex Hospital Medical School in London, England. The post had responsibility for steroid endocrinology in the Department of Clinical Chemistry but allowed research and development with a number of eminent clinicians. I collaborated in research for the early use of in-vitro fertilisation (Professor Howard Jacobs), paediatric endocrinology (Professor Charles Brooks) and hypertension (Professor JDH [Willie] Slater) in the illustrious company of Professors Roger Ekins who had developed hormone binding assays akin to the immunoassay developed by Rosalyn Yallow and Sol Berson. Aldosterone had been discovered at the Middlesex Hospital in 1953 by Jim and Sylvia Tait. Earlier work by E.C Dodds between 1922 and 1952 had looked at many endocrine problems including the use of stilboesterol to treat certain cancers. Dodds had shown the feminisation of chickens through administration of reduced phenanthrene (an early endocrine disruptor). The feathers and a watercolour of the results were preserved in a frame on the wall of the Head’s office as a reminder to us.
The Middlesex Hospital was closed in 1988 in a reorganisation of medical schools but I continued steroid research in University College London Hospital and took more responsibility for clinical liaison and Clinical Chemistry department management. Research into the molecular genetics of steroidogenic enzymes started in my laboratory in 1988.
Several research projects examined the safety of inhaled steroids (ICS) with respect to effects on the hypothalamic-pituitary-adrenal axis. In children taking inhaled corticosteroids, growth was suppressed. Blood samples from the children were taken at regular intervals throughout the night to see if growth hormone secretion was affected. Using these samples the pattern of cortisol release showed that cortisol pulsed at 90 minute intervals, the peaks increased in amplitude with the last and highest peak being around 0800h. ICS were found to suppress the pattern of cortisol, the number of peaks lost related to the dose of ICS. This work revealed to me several important facts about the HPA axis. The diurnal rhythm of cortisol is really an ultradian rhythm. Further studies showed that not all subjects peaked at 0800h, the variation was from 0600 to 1000h. These data explain the range of cortisol concentrations at 0800h between 200 and 800 nmol/L because the pulsatile patterns of individuals are out of phase. A collaboration with Peter Hindmarsh at GOSH has led to use of an insulin pump to deliver hydrocortisone subcutaneously in a more physiological manner. Originally tested in patients with congenital adrenal hyperplasia it is now being used by patients with Addison disease and hypopituitarism.
In collaboration with Willie Slater we pursued experiments on low dose ACTH tests (1 microgram instead of 250 micrograms) we found a dose of 1 microgram per metre squared of body surface gave a peak comparable with that achieved at 30 minutes from 250 micrograms. When precursors were measured the peaks were earlier then 30 minutes. Although we reported this in 1998, the protocols in the literature have not refined the test to include samples earlier than 30 minutes and the literature is now very confusing.

The book covers important advancements in the field and is a valuable addition in the literature addressing all existing knowledge gaps. I hope the book will be a “must have” reference for pathologists, laboratorians, endocrinologists, analytical/clinical chemists and biochemists.
In 1999 I became a Consultant Clinical Scientist in and Reader in Steroid Endocrinology. In addition to reporting quantitative results I was required to offer interpretation of the results and advice for further investigations. This was possible from my experience in the investigations of disorders of the adrenal cortex and gonads. Comprehensive reference ranges for steroids were established and validated for all of the tests. Research in the unit covered the validation and use of mass spectrometry in steroid analysis for disorders of sex determination, adrenal diseases, polycystic ovary syndrome, safety of corticosteroids in treatment of asthma, links between birthweight and cardiovascular risk, and the enterohepatic circulation of steroids.
I was successful with many research grant applications to fund research in the unit such as a study peripheral 21-hydroyxlase; adrenal function in HIV, children with asthma, children in relation to birthweight (Avon Longitudinal Study Parent and Child -ALSPAC) and osteoporosis from a vegetarian diet. I was very disappointed that an application in 2002 for funds from a government scheme entitled “New and Emerging Analytical Technology” (NEAT) to purchase an LC-MS/MS system was declined because it was not “new”!
I was scientific adviser to UKNEQAS for quality control of immunoassays to improve steroid accuracy then paediatric investigations. I served on the Editorial Board of Clinical Endocrinology and two working parties for Lawson Wilkins Pediatric Endocrine Society with the European Society for Paediatric Endocrinology that produced guidelines on congenital adrenal hyperplasia and newborn screening. I was Treasurer of the British Society for Paediatric Endocrinology and Diabetes (BSPED) for 12 years. An EQA scheme for urinary steroids was operated globally from UCL with the collaboration of the Dutch Foundation for Quality in Clinical Chemistry (SKML).. I was an Associate Editor of the Annals of Clinical Biochemistry and a member of the Independent Review panel for UK Anti-doping. I am now an Honorary Senior Research Associate at the Institute for Women’s Health at University College London.
EN: Tell us a little about the process of writing the book.
I started with the 170 papers and 19 book chapters that I had written and lectures given to students and conferences so writing the text of the book was not difficult. The biggest problem was getting permissions for copyright content, this was a retrospective exercise. I would now advise any book author to collate that information whilst writing. The book ended up as a 988 page monster from nearly 320,000 words, unfortunately as a pa er- back. There are more than 730 figures and 120 Tables to enhance comprehension of the wide-ranging and often complex material. There are many unanswered questions giving many opportunities for further research by keen clinicians and laboratorians.
The book was partly written in the year 2020/2021 when the world was struck with a pandemic through a SARS virus (Covid 19). Because of health problems I was placed by the UK government into lockdown which meant not being able to leave the house for nearly 24 months to shield from exposure to Covid. The time enabled me to focus on writing the book in a period when some people almost struggled with the purpose of life when confined to the house.
EN: Can you point to an example or an anecdote of a clinician being stumped by an abnormal lab result, and how this book would have helped alleviate that confusion?
JWH: I have many examples where a clinician is stumped by a laboratory result. Immunoassays have revolutionized endocrinology but are prone to interferences that may alter tests results, putting patients at risk for misdiagnosis. An immunoassay (IA) is an analytical test method in which analyte (hormone) quantitation is based on signal responses generated as a consequence of an antibody–antigen interaction coupled with a detection system that generates a signal response from a label (e.g., radioisotopic, enzymatic, fluorescent, or chemiluminescent). The combination of an easily detectable signal and a protein which binds with high affinity to an analyte is principle to all immunoassay methods. Early immunoassays (IA) used polyclonal sera from animals (sheep, rabbits) injected with hormones to create antibodies to the hormone. Blood samples from people in contact with the animals have antibodies that can react in IA if they need laboratory blood tests. Anyone who handles mice is exposed to mouse proteins and can also generate antibodies in their blood (HAMA). Mice cells are used in the laboratory to create monoclonal antibodies with many uses in medicine. Immunoassays for proteins are often based on two antibodies that react with different areas of the protein. These are called sandwich assays but HAMA can form a bridge between the two antibodies and more of the usual signal is generated giving the impression of elevated hormone concentrations. Some people also have auto-antibodies (e.g. rheumatoid factor) that react like HAMA in IA (heterophilic reaction).
Many immunoassay manufacturers exploit the extremely high affinity of biotin for streptavidin in their assay design architectures as a means to immobilize and detect analytes of interest. Since the biotin–(strept)avidin interaction is one of the strongest known non-covalent interactions in nature, avidin and its analogues have been extensively used as probes and affinity matrices for a wide variety of applications in endocrinology and elsewhere. Biotin has gained commercial popularity for its claims on benefitting hair growth since it is an essential factor for enzymes in hair roots. Many hormone assays use biotin–(strept)avidin-based regents but are susceptible to interference with biotin. Excess biotin from the sample can inhibit immune complex separation by binding to the binding sites of (strept)avidin usually reserved for the capture or detection of the analyte. Unusually high concentrations of circulating biotin can be due to the excessive intake of supplements containing biotin. The impact of the observed interference is dependent on the concentration of biotin, the hormone being measured, and the architecture of the affected assay causing falsely low (non-competitive) or falsely elevated (competitive) results. In a sandwich assay the resulting signal is reduced, leading to falsely decreased results. In a competitive assay, ruthenium labeled antigen competes with analyte for their biotinylated antibodies. With the presence of analyte, unlabeled analyte competes with ruthenium labeled antigen for binding with the antibodies. The signal for measurement is inversely proportional to the concentration of analyte. Consequently, biotin interference may give the falsely elevated results.
EN: Any result not consistent with the clinical findings should be discussed with the laboratory.
JWH: In a year of Olympic Games I am reminded of my role in steroid abuse in sport. In 1994 a female British athlete was sent home from the Commonwealth Games because she had been found in a previous drug test to have a raised testosterone shown by GC-MS analysis of her urine and accused of taking performance enhancing drugs. I found that the urine sample had been left outside the anti-doping laboratory for 3 days in Lisbon, Portugal in mid-summer. I proposed that the testosterone in the urine had been produced by bacterial action of natural steroids in the urine. She lost her conviction but on appeal proof of the bacterial hypothesis was presented and she was found innocent of testosterone abuse. Samples in sport are collected without the addition of preservatives as would be the case with clinical samples.
I then acted as expert witness in several cases of Nandrolone (19-nor testosterone) abuse that turned out to be due to contaminated nutritional supplements. I hope the Olympics this year is not tarnished with the use of performance enhancing drugs. Drugs called selective androgen receptor modulators (SERMS) seem to be common culprits in recent years. My book deliberately avoided a discussion of performance enhancing steroids.
It was always thought that licorice causes hypertension because it acted like aldosterone. We now know that licorice inhibits an enzyme that oxidises cortisol in the kidney tubules allowing cortisol to act on the aldosterone receptor.
Fortunately for me steroid assays based on mass spectrometry are not subject to these interferences although the ability of chromatography to separate components of the test must be confirmed. MS looks at the molecular weight of the analyte so steroids of the same composition must be apart in the chromatography from the steroid under investigation. Clinicians see MS tests as the gold standard but the laboratory must prove that to be the case.
EN: Finally, what do you hope readers take away from your book? Why should they pick it up?
JWH: I hope this book should become the “go-to” for answers to questions around steroids. These hormones and their metabolites, once considered inert, are now all playing important pivotal functional roles. My professional journey provided me with unmatched broad experiences of steroids in clinical practice that enabled me to write the book for others to benefit. Thank you for giving me the opportunity to talk about my book.