A new study seeks to establish a clinical guideline to quantify the risk of metastatic lymph nodes in thyroid cancer patients. The findings should go a long way to help ease the mind of the patients…and the physicians.
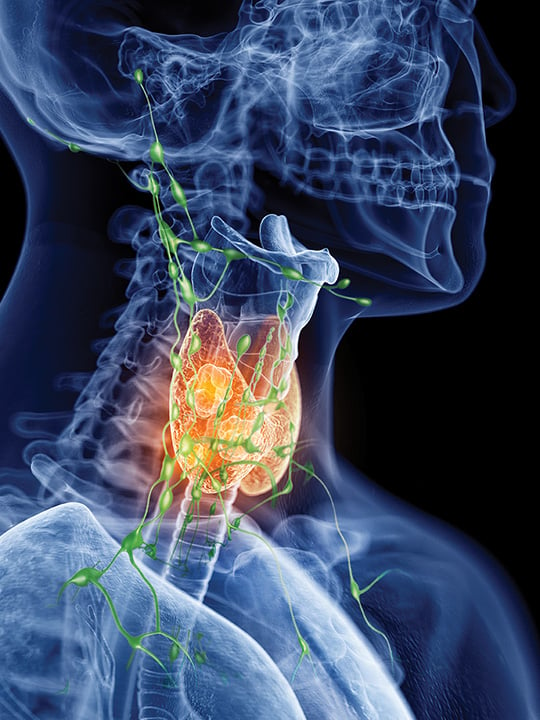
With thyroid cancer incidence on the rise, especially papillary thyroid cancer, surgical tumor resection is a critical component of the overall treatment plan, which might also include one or more of several adjuvant treatment options such as concomitant lymph node (LN) dissection.
The American Cancer Society notes that although an estimated 62,450 new cases of thyroid cancer will be diagnosed in the U.S. in 2016, fortunately, the death rate (about 1,980 deaths from thyroid cancer) has not increased alongside incidence. Nevertheless, five-year survival rates for stage IV papillary thyroid cancer remain at only about 51%, and lymphovascular invasion is a key risk factor for occult, recurrent, or persistent disease.
With standards yet to be established regarding the number of LNs a surgeon might remove to help determine the existence of occult disease — in addition to variations in clinical management — thyroid cancer patients may be undergoing unnecessary or even inappropriate treatments that themselves carry risk for debilitating complications.
Lymph Node Assessment Model
In “How Many Lymph Nodes Are Enough? Assessing the Adequacy of Lymph Node Yield for Papillary Thyroid Cancer,” published in the Journal of Clinical Oncology, a team of researchers from the Duke Clinical Research Institute and the Duke Cancer Institute in Durham, North Carolina, including Julie A. Sosa, MD, MA and Terry Hyslop, PhD, set out to provide as definitive an answer as currently possible to the question posed in the title of their pioneering study.
“…Endocrinologists and their patients can make decisions about the need for other treatment based on good pathologic evidence. Knowing how many lymph nodes would need to be assessed to truly be certain of the risk of occult disease can help them with dynamic staging, adjuvant treatment choice, and intensity of follow-up.” – Terry Hyslop, PhD, Duke Clinical Research Institute, Duke Cancer Institute, Duke University, Durham, N.C.
From previous investigations, the team found that the median number of LNs removed is two, but this practice is largely arbitrary. Because occult disease is, by definition, not readily identifiable with existing imaging studies, determining whether it exists can currently be done only by pathologic examination. “It is quite common to have the thyroid removed along with an incidental lymph node,” explains Sosa, “. . . [but] is one random lymph node enough? Are two enough? Five? No one really knew. We embarked on this study to better inform physicians and patients about the adequacy of LN evaluations and what that may mean from a risk-benefit perspective for the patient.” Retrospectively analyzing National Cancer Database data from 38,653 patients diagnosed from 1998 to 2012 with localized ≥1-cm papillary thyroid cancers who underwent thyroidectomy with one or more LNs surgically examined, researchers used a mathematical model in a stepwise fashion to first estimate risk of false-negative LN dissection; second, prevalence of true-positive LNs; and, finally, risk of occult disease.
Clinical Decision-Making: It’s a Team Effort
Although the risks of central lymphadenectomy are not typically life threatening and absolute contraindications do not exist, complications can certainly negatively impact patient quality of life; therefore, careful reckoning of risks versus benefits is critical. These risks, explains Sosa, include increased risk of transient or permanent hypoparathyroidism and hypocalcemia, necessitating calcium and vitamin D supplementation by mouth, as frequently as every four to six hours, as well as dysfunction of the recurrent laryngeal nerve, resulting in the inability to speak (or even breathe, which could require a tracheostomy), and the external branch of the superior laryngeal nerve, resulting in a change in volume and pitch of voice and the inability to sing or speak loudly.
Thus, in a patient with a tumor not likely to have metastasized, knowing prior to surgery what that risk most likely is would prove an invaluable tool for designing the ideal treatment plan. Says Sosa: “There is a quandary faced by the entire healthcare team — for the surgeon, whether to take the lymph nodes out; for the endocrinologist, whether to give radioactive iodine, in part based on the information obtained about lymph nodes during surgery; and for the patient, whether the information and treatment will result in better survival. We are trying to quantify the risk.”
Patient input is particularly important in this context. “If a patient is anxious about the risk of harboring occult metastases, evaluation of more lymph nodes can bring peace of mind,” Sosa explains. “However, if a patient is very risk averse, then surgery can be tailored accordingly.”
Potential Clinical Guidelines on the Horizon
Quantify risk they did, concluding that in a patient with a 1–2-cm tumor (T1b disease) removing six LNs that test negative would suffice to provide 90% confidence that the cancer has not metastasized. The number of LNs needing to be removed rises to nine if the tumor is 2–4 cm (T2 disease) and to 18 if the tumor is >4 cm and/or is associated with minimal extrathyroidal extension (T3 disease).
“We embarked on this study to better inform physicians and patients about the adequacy of LN evaluations and what that may mean from a risk-benefit perspective for the patient.” – Julie A. Sosa, MD, MA, Duke Clinical Research Institute, Duke Cancer Institute, Duke University, Durham, N.C.
“We do not know the exact probability for each unique patient, but our conclusions are based on patterns within a very large set of data,” Hyslop says. “This information can help surgeons tailor their resections. The data might help the pathologist be more fastidious in finding lymph nodes in the specimens. Then endocrinologists and their patients can make decisions about the need for other treatment based on good pathologic evidence. Knowing how many lymph nodes would need to be assessed to truly be certain of the risk of occult disease can help them with dynamic staging, adjuvant treatment choice, and intensity of follow-up.”
– Horvath is a freelance writer based in Baltimore, Md. She wrote about the link between endocrine-disrupting chemicals in utero to breast cancer in adulthood in the October issue.


