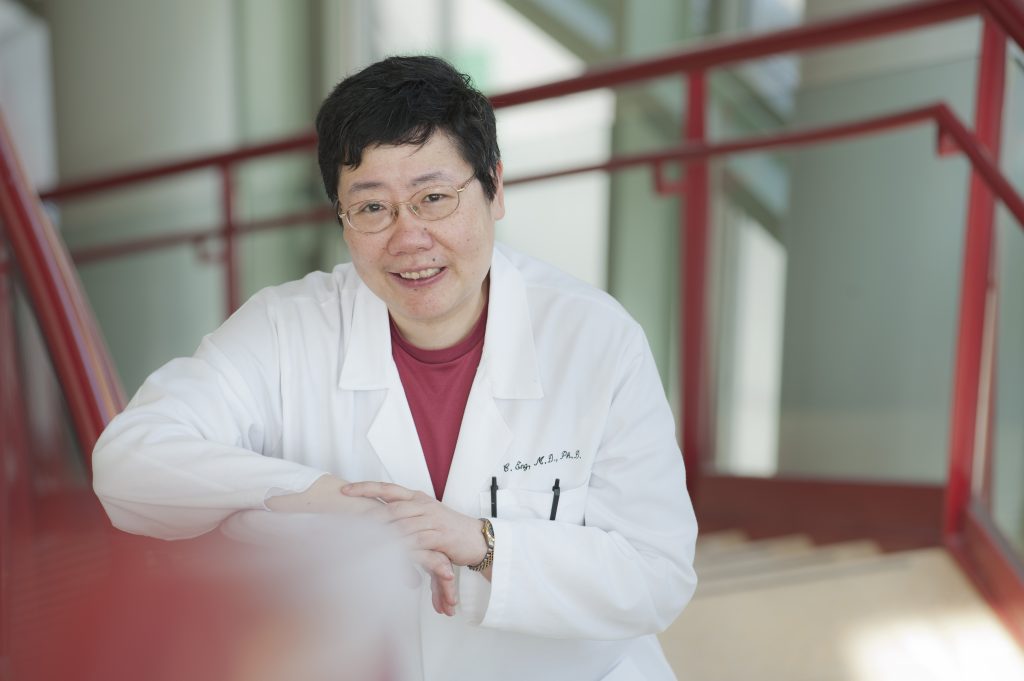
Charis Eng, MD, PhD, from the Cleveland Clinic, discusses her research of tumor suppressor genes, endocrine neoplasias, and why an accurate family history is so important to determine when a cancer screening should be performed.
The American Cancer Society’s Medal of Honor recognizes individuals who have made the most valuable contributions in saving more lives from cancer. One of the 2018 recipients, Charis Eng, MD, PhD, of the Cleveland Clinic, is no stranger to the endocrine community and was honored for her study of tumor suppressor genes and the understanding of hereditary predisposition and treatment for several types of cancer, including those endocrine related.
Endocrine News spoke with Eng to learn more about the work that earned her Medal of Honor accomplishment.
Endocrine News: What were your first thoughts when you heard about your Medal of Honor for Clinical Research?
Charis Eng: It was a tremendous honor and I had all sorts of emotions flooding in and asking, “Can this be true?” It was such a lovely surprise because with a lot of these awards, the intended recipient helps put in the nomination, but I didn’t with this one. And so, someone anonymously nominated me and that is the greatest surprise of all.
EN: A simple explanation of your research is that humans have about 24,000 genes and about six bad ones that can predispose us to serious illness. The goal is to screen for these genetic mutations and identify a patient’s cancer risk. Your lab is creating a road map for patients to alert them of their increased risk so they can make better decisions about their health and lifestyle. How close are patients to being able to get a roadmap of their predispositions?
CE: Let’s step back. We already have a roadmap if only clinicians have the time to take a good family health history. A good family history can provide that first inkling of, “Could I be at increased risk of something that’s running in my family?” The truth of the matter, of course, is that non-genetic clinicians don’t have the time. The family health history is sacrificed because clinicians are sitting in front of a patient who has other illnesses that might need immediate care. So, of course that’s the problem — it’s reactive medicine versus proactive medicine.
I think there are some of the greatest minds studying thyroid cancer, but it’s just such a complex field that it’s taking a very long time. And until very recently, the funding bodies have said, “Nobody dies of thyroid cancer. We don’t care.”
But, because of mine and other’s research, there are now 59 clinically actionable genes and soon to be 71, that are in the American College of Medical Genetics and Genomics guidelines. The guidelines say that if incidentally any of these are found, whether as a screen or in research, they have to be confirmed in a CLIA/CAP certified lab in the setting of genetic counseling and these have to be actioned.
And since I study endocrine neoplasias, I have defined the risk of various endocrine neoplasias. For example, I am most known for finding the PTEN gene, which when altered leads to a very high risk of breast, thyroid, endometrial, and other cancers. I name those three because they are the highest risk and they are “endocrine organs.” So, if there’s an alteration in the PTEN gene, it’s an 85% lifetime risk of female breast cancer. It’s a 35% lifetime risk of thyroid cancer and an 28% risk of endometrial cancer, and endometrial cancer is normally about a 1% – 2% risk. But because of our research, we know when the age of risk begins and how high the risk is in a lifetime.
So, this is where this type of research can be translated to practice guidelines. We know when to begin clinical screening or enhanced surveillance because it is starting earlier and more often. For instance, we’ve found that the youngest onset of thyroid cancer associated with germline PTEN alterations is six years old. And so, the original practice guidelines were, “We could start screening in the teens.” And when our research came out, we said, “No, we cannot.” And our study, replicated twice independently, formed the basis of altered practice guidelines. So, the moment the doctor finds a PTEN mutation, you begin thyroid ultrasounds annually immediately upon that genetic diagnosis, so this is how our work has changed practice.
EN: You’re also the editor-in-chief of the journal Endocrine-Related Cancer. Regarding submissions, what’s the more prolific area of research now?
CE: I would say thyroid cancer research is prolific but not prolific enough, because if you look at thyroid cancer as a whole versus all the other endocrine neoplasias, the knowledge is far behind. Not because we’re not good — I think there are some of the greatest minds studying thyroid cancer, but it’s just such a complex field that it’s taking a very long time. And until very recently, the funding bodies have said, “Nobody dies of thyroid cancer. We don’t care.” And that’s not true because when it’s advanced thyroid cancer, you’re wringing your hands and wondering, “Now what?” and there’s no recourse. So, I think more people need to work harder.
The moment the doctor finds a PTEN mutation, you begin thyroid ultrasounds annually immediately upon that genetic diagnosis, so this is how our work has changed practice.
EN: Can you share more about the team at your Eng Lab?
CE: I started the lab at the Dana-Farber Cancer Institute in 1995 and it was just me and four other people. I’ve been at the Cleveland Clinic for 13 years where I founded the Genomic Medicine Institute and its clinical components. We have the most comprehensive practice of medical genetics and genomics in the country. My lab runs anywhere from 12 to 18 people and it swells in the summer when I take summer medical or undergraduate students, and even high school students, because I believe strongly in having a pipeline of our next generation.
Read more about Dr. Eng’s research at www.lerner.ccf.org/gmi
—Glenda Fauntleroy Shaw is a freelance writer based in Carmel, Ind. She is a regular contributor to Endocrine News.

