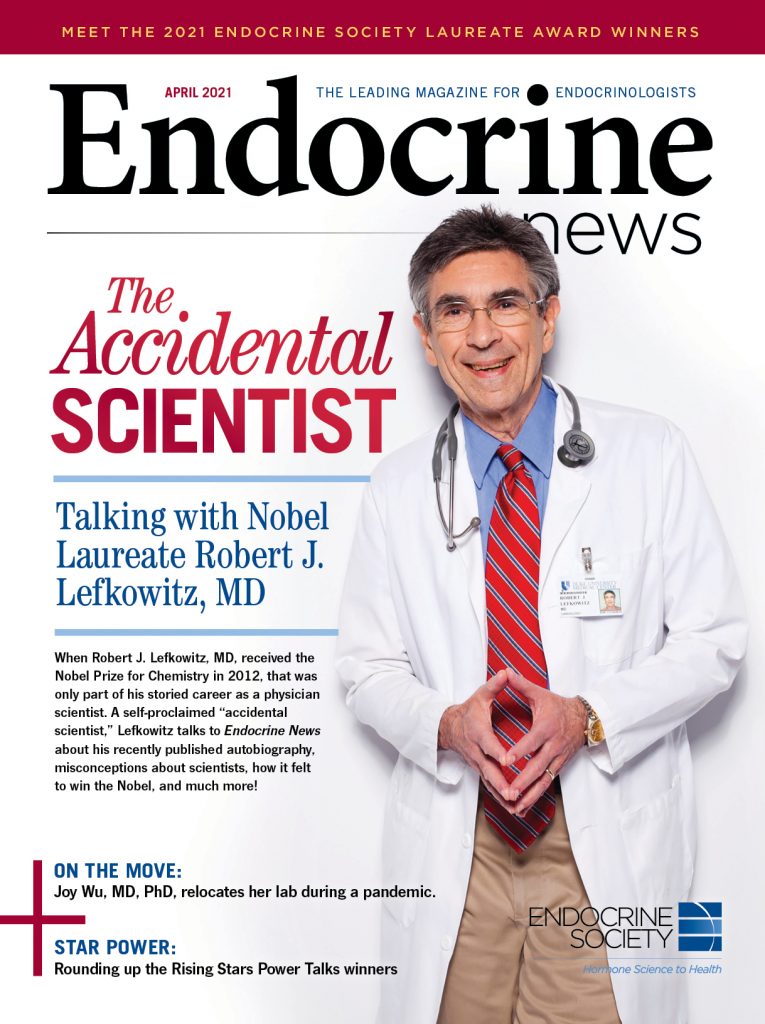
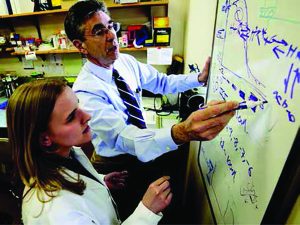
When Robert J. Lefkowitz, MD, received the Nobel Prize for Chemistry in 2012, that was only part of his storied career as a physician scientist. With a new book on the shelves – and online shopping carts – Lefkowitz talks to Endocrine News about misconceptions about scientists, what inspired him to write a book, and how it feels for a self-described “accidental scientist” to receive a Nobel Prize.
What do you do when you’ve reached the pinnacle of your field? Where do you go from there? For Robert J. Lefkowitz, MD, James B. Duke professor of medicine and investigator with Howard Hughes Medical Institute at Duke University – as well as Nobel Laureate – the next logical step is to publish a memoir, especially if you can tell a tale the way Lefkowitz does.
Lefkowitz’s book A Funny Thing Happened on the Way to Stockholm: The Adrenaline-Fueled Adventures of an Accidental Scientist, hit shelves in February, a collection of stories that recounts Lefkowitz’s journey from serving in the “Yellow Berets” to winning the 2012 Nobel Prize in Chemistry for – along with Brian Kobilka, MD, professor and chair of molecular and cellular physiology at the Stanford University School of Medicine – his work on G-coupled protein receptors, which about a third of all drugs now target.
Endocrine News will run an excerpt from A Funny Thing Happened on the Way to Stockholm as well as some of Lefkowitz’s thoughts on the plight of physician-scientists today on our this site later this month, but here, edited for length and clarity, is our conversation with Lefkowitz, about the path that led him from cardiologist to reluctant researcher to Nobel Prize winner, and how his memoir comes at a pivotal moment in medical science.
Endocrine News: Tell me a little about the experiences that led you to becoming an “accidental scientist.”
Robert J. Lefkowitz: I used the term “accidental scientist” because I had no intention of being a scientist. I had decided by the time I was eight years old that I was going to be a doctor, and I never wavered from that. I went straight through Bronx High School of Science; my classmates wanted to be physicians. That was of course the middle-class Jewish dream, or stereotype, in the 50s, “My son the doctor.” There had never been a doctor in my family. It was an immigrant family of relatively modest means.
I went through Columbia College, Columbia Medical School, and then house staff, internship and residency at Columbia. I was always very interested in science. I loved my science courses, especially anything to do with biochemistry. But that said, I didn’t envision myself actually practicing science. I just liked knowing it, and although I had many opportunities, especially in college, and medical school, to do research electives I never availed myself of a single one.
In college, I would always use those periods to take things like philosophy and sociology. In medical school, I always did clinical rotations. So then, something happened, a cataclysmic event, which would alter the course of my entire life and career, and that of so many others, the Vietnam War.
The war was raging in the ’60s. I graduated medical school in 1966. At that time, there was a lottery draft for all men over 18. That meant it was a lottery, but not for physicians — there was just a draft. You were drafted at the time of your graduation from medical school, and then you were given an automatic one- or two-year deferment to gain some clinical experience as an intern, or a resident, and then you went in, Army, Navy, Air Force, whatever.
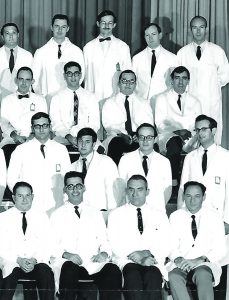
stateside rather than heading to Vietnam. In this 1968 U.S. Public Health Service photo of the staff of the National Institute of Arthritis and Metabolic Diseases (as it was then known), I’m in the third row, second from the left, and
joined by two fellow Yellow Berets who would later go on to win Nobel Prizes: Harold Varmus (top row, third from left) and Mike Brown (second row, second
from left). PHOTO COURTESY OF ROBERT J. LEFKOWITZ
Many felt the war was immoral, some felt it was illegal, but most of my colleagues and friends like myself did not want to support this war by serving in Vietnam. The problem was there were very few legal ways around it. One of the few was to gain a commission in the United States Public Health Service. The United States Public Health Service was then considered one of the military branches. Most of their members were officers serving within the United States, and in particular they had assignments available at the NIH, the CDC, and several other research institutions. But as you can imagine these commissions were extraordinarily competitive to get. I was always had very high academic standing, good recommendations, top schools, so I got into the program, and was assigned for two years at the NIH, not because I specifically wanted to do research, but for the reasons that I explained.
My entire generation of academic physician scientists came out of that program. And to give you a sense of the remarkable success of that program, commonly known as “The Yellow Berets” [a derisive take on the Green Berets – yellow to imply cowardice], in my class, four of us went on to win the Nobel Prize. Myself, Michael Brown, Joe Goldstein, and Harold Varmus. And there was one other guy in the group you may have heard of, who did okay for himself even though he didn’t win a Nobel Prize, Tony Fauci. Tony was in our class. We all knew each other. We’re all good friends to this day.
You can argue that for most of us we were accidental scientists. I’d have to talk to them to find out if that’s true, but absent that experience who knows that any of us would’ve done.
EN: That’s quite the pivot from cardiologist.
RJL: I served [at the NIH] from 1968 to 1970, and it did not initially go well, and that was difficult for me because I had never really failed at anything in my life, much less in a sustained way, but here I was after a year of the hardest effort that I could put forth and I was nowhere with my project. That convinced me that by no stretch of the imagination research was something that I wanted to make part of my career, and so I made plans at that point, at the one-year mark, to finish my clinical training a year later at the Mass General Hospital in Boston where I would do a final year of senior residency to be followed by two years of cardiology fellowship.
“I realize the whole ‘publish or perish’ thing, and you’ve got to get grants, but it’s worth bearing in mind that if you really want to make important discoveries you have to work on challenging problems.”
As luck would have it, during my second year at the NIH things began to click, and by the time I finished there I had been able to write with my mentors my first few papers. I’d gotten a taste of what success is like in research, and I was starting to like it, and I was importuned by my mentors to stay on for additional training. They said, “You have really got a hot project now.” But I was not that convinced, and I went off to the MGH.
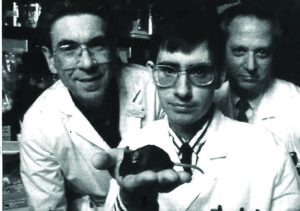
I threw myself with gusto into the clinical work, but at the six-month mark at the Mass General I had a real epiphany because I realized I had this feeling that something was missing from my life, and I realized it was the research, the day-to-day challenge of planning and doing experiments, making up hypothesis, the whole bit.
EN: The creativity you talk about.
RJL: I realized that I had this creative spark or instinct, which was just not being met by my clinical duties, and so I found a mentor, quite a noted scientist, and also chief of the cardiology division, and persuaded him to let me begin doing experiments in his lab part time while I finished my clinical training, and for the remaining two and a half years that I was there I continued to do just that.
EN: Your Nobel Prize work, the discovery of GPCRs, they’re at the intersection of everything, especially in endocrinology.
RJL: When I went to the NIH, I was assigned to two mentors, Jesse Roth and Ira Pastan. They both were card-carrying endocrinologists, and I was assigned to the Clinical Endocrinology Branch. The funny thing about that is we split our time about 20% doing clinical work, and 80% doing research. The clinical time was every bit the equivalent of an endocrine fellowship.
Jesse and Ira had it in their head that hormones worked through mystical entities called receptors for which there was no proof at all, and in fact the idea was very controversial, but it was an idea right at the intersection as you say of pharmacology, cardiovascular medicine, endocrinology, etc.

festivities, as seen as I received the Nobel Medal from King Carl XVI Gustaf.
PHOTO COPYRIGHT © NOBEL MEDIA, PHOTO BY ALEX LJUNGDAHL.
To pharmacologists, and I think to endocrinologists, receptors were just some general pattern of forces on a cell that allowed hormone and drug molecules to interact. I came to the conclusion really for two complimentary reasons to make the so-called beta adrenergic receptor the target of my studies. One, I was an aspiring young academic cardiologist. I wanted to work on something relevant to cardiovascular medicine, and two, I had certain technical requirements, lots of analogs to work with. Those things seemed to come together on the beta-adrenergic system, and so I opted to work on that, and here I am just 50 years later, and I still work on it.
EN: How big was the buzz around the lab when you found out you won the Nobel Prize in Chemistry?
RJL: It was amazing. I had been touted for the Nobel for up to 20 years. By touted I mean people were saying, “You know, Bob, you might win this thing,” and it didn’t happen, and it didn’t happen, and it didn’t happen.

my family (left to right): Joshua Lefkowitz, David Lefkowitz, his wife Michelle, Lynn Lefkowitz, me, Mara Lefkowitz Mack, Cheryl Herbsman, Mara’s boyfriend (now husband) Eric Mack, Maya Herbsman, Jonah Herbsman, Wade McCollum (Noah’s husband), Oded Herbsman (Cheryl’s husband), Noah Jordan, and my cousin Ellen Danziger. PHOTO COPYRIGHT © NOBEL MEDIA, PHOTO BY ALEXANDER MAHMOUD.
So then, in 2012 it’s Nobel announcement week, and as you know they give the prizes in a set order, Monday they announce medicine, Tuesday’s physics, Wednesday’s chemistry. Monday has come and gone, and they give the prize for induced pluripotent stem cells. I thought that was great. Then on Wednesday morning at five o’clock the phone rings, and I sleep with earplugs so I don’t hear it, but my wife picks it up, and gives me a poke in the ribs, and she says “There’s a call for you from Stockholm.
The day was absolutely nuts. I have five children spread across the country, and I was only able I think to personally inform two of them because I got the call at 5:00am, and they said that they’ll make the announcement at 6:00, which is 11:00 Stockholm time, and they said you can’t tell anybody, not even family until we make the announcement, and no sooner had they made that announcement at 6:00 than my phone went crazy. Newspapers were calling, and it was amazing. When I got to my office it was filled with people, not just from my lab, but passers by, and anybody who was in the building stopped in. There were balloons. There was a big news conference.
It turned out to my surprise I was the very first Nobel Laureate ever to be at Duke University. They really pulled things together, and by 4:00 that afternoon there was a beautiful catered reception at a big hotel across from the campus with hundreds of people there that they had organized in the course of basically eight hours.

enjoyable chat with President
Obama before heading to Stockholm
for the Nobel festivities in 2012.
PHOTO COURTESY OF ROBERT J. LEFKOWITZ
In contrast, I shared the prize with one of my former trainees, Brian Kobilka, who now is a distinguished professor at Stanford. At Stanford, Nobel Prize winners are thick on the ground. In the history of the university I think they’ve had 25 Nobel Prize winners or something like that, compared to one at Duke, (at the time) so they have a protocol in place, and within an hour of Brian getting the phone call there was a team from the public relations office at his home and they handled all the incoming calls, the press, and everything that was going on.
EN: That’s got to be an incredible feeling. Now to your book. What prompted you to write it, and tell me about the writing process.
RJL: It’s a good story. As you have learned already during our short time we’ve known each other I’m a bit of a raconteur. I especially love stories with a humorous aspect to them, and anybody who’s trained with me knows that I love to tell stories, and for years people have been trying to get me to write a book with some of my stories. I don’t think I ever would’ve done it. Just too much going on.
“The subject of training physician scientists is near and dear to my heart. It’s sad, but today in surveys if you ask physicians, ‘Does research play any role in your career? Do you do any research at all of any kind?’ Only about 1.5% answered yes, so that means that 98% to 99% of all physicians do no science, no research, at all. And the problem with this is, where’s the next Tony Fauci going to come from?”
One day a couple of years ago one of my former postdocs, Randy Hall, had come up as he does every couple of years to attend a Duke basketball game with me. He’s an ardent fan, and I have season tickets. We were having dinner before the game, and of course I was regaling him with stories, and he says, “Bob, you really have to write these things up.” I said, “Well, I’m not going to.”
He says, “Look. Let me pitch you an idea. Do you know the book, Surely You’re Joking, Mr. Feynman!? Why don’t we model it on that? We’ll start talking every week. I’ll record it. You tell me your stories. I’ll write them up. You edit them, and we’ll put them into some sort of narrative framework, and let’s see if we can come up with a book.” Over the course of a year I would say we spoke two hours a week, he recorded everything, so he had about 100 hours of my storytelling, and we went chronologically. I would prepare for each session by just trying to think of all the stories I’m always telling from childhood, teenage years, and just going through it.
And then, we organized them, we found ourselves a very good literary editor, and a nice publisher, and the book was published [on February 2].
EN: One thing that stuck out to me is how you talk about your trepidation when you started as a researcher, and I wonder if you have any advice for these young researchers who may feel the same way, that they had a calling to be a clinician, but now they might start whetting their appetite for research, or they have this hidden love for it. What kind of advice do you have for young researchers?
RJL: A number of years ago, I was in my office over the Christmas holiday break going through a ritual which I have done virtually throughout my career. During that week, Christmas and New Years, I’d sit for several hours by myself, and I’d think about all the projects going on in the lab.
I was working on that, and this young physician scientist, good guy, comes in. He says, “What are you doing, Bob?” I told him, and he said, “Oh, that’s not a bad idea.” I said, “How was your past year? How are your projects doing?” He says, “Great.” I said, “No kidding. What percentage of what you’re working on is panning out?” He says, “Almost everything, at least 80%, maybe 90%.”
“No kidding.” I said, “That is a good year.” He said, “What about you?” I said, “It’s right around 20%, which is about where I’d like it to be.”
He said, “What are you talking about?” I explained to him that reflexively if I get to the end of the year and anything 50% or more of what I’ve got listed seems to be working I conclude that I am dogging it, that I must be taking on things that are not as challenging as they should be, and I really think about that, so if 20% of my projects are moving forward in some way or another I’m quite happy.”
He was initially surprised, but I can’t tell you how many times over the last decade he has thanked me for that conversation. He told me it put his whole research program into a different orbit than he had been in, and to tell you the truth his research has really deepened and improved over these years. That’s one thing I would talk to young aspiring scientist about. I realize the whole publish or perish thing, and you’ve got to get grants but it’s worth bearing in mind that if you really want to make important discoveries you have to work on challenging problems.
EN: Don’t be afraid to fail.
RJL: Absolutely. Failure is just an essential element in what we do.
EN: I’m given to understand that you have some prescriptions for this shortage of physician scientists you’re seeing. As you say, your career path was shaped by things that can’t be repeated, like the Vietnam War.
RJL: The subject of training physician scientists is near and dear to my heart. It’s sad, but today in surveys if you ask physicians, “Does research play any role in your career? Do you do any research at all of any kind?” Only about 1.5% answer yes, so that means that 98% to 99% of all physicians do no science, no research, at all. And the problem with this is where’s the next Tony Fauci going to come from?
In a sense, it’s a vicious cycle in that as the number of physician scientists has declined there are fewer and fewer role models for medical students to see. In my day, they would see people like myself, or the people I just mentioned, Mike Brown, Joe Goldstein, and Tony Fauci on rounds, people who knew one end of a stethoscope from another, but who could also talk to you about the biochemistry and physiology of the disease processes they were seeing before them. Today there’s this lack of role models, and to the extent that there’s a lack of role models fewer and fewer people go in for this type of career.
The training has gotten longer and more expensive, and it’s hard to stick with it because obviously if you’re going to do both it takes more years of training, so there’re all sorts of problems. And so, we’re hoping to counter this to a certain extent. A small group of us have formed a non profit organization called the Physician Scientist Support Foundation (PSSF). Right now, we’re focusing our energies on trying to develop programs for medical students who’d like to take a year out of their medical school curriculum and spend it in a laboratory.
EN: What do you hope readers take away from your memoir? Why should they pick it up?
RJL: What I’m hoping people take away from the book is just what a joy it is to have a career as a physician scientist in my case, or as a scientist. I think several people who have looked at the book talk about what comes through is the joy of discovery, and the joy of the hunt, for scientific knowledge, and also I think the book for lay people I hope it will humanize the people who are doing science. I think a lot of lay people look at scientists as being some stuffy, dry sort of characters but if they get to know me at all, which I think they will through this book, they will see that I’m having a very good time, so it’s infectious. People in my lab who look back on their experience often tell me “I had more fun during the years I was in your lab than I’ve had at any point since”, and I take a lot of pride in that.
— Bagley is the senior editor of Endocrine News. In the February issue, he wrote the cover story on how endocrine nurses have become more essential than ever during the COVID-19 pandemic.
— Captions by Robert J. Lefkowitz, MD