
Since the first, all-virtual ENDO 2021 stemmed from the lingering effects of the COVID-19 pandemic, Endocrine News presents an overview of the research that specifically addressed how the virus affects patients with common comorbidities. These studies looked at COVID-19’s effects on patients with obesity, hyperglycemia, adrenal insufficiency, and a lack of vitamin D, and provide a better understanding of this new and often devastating phenomenon.
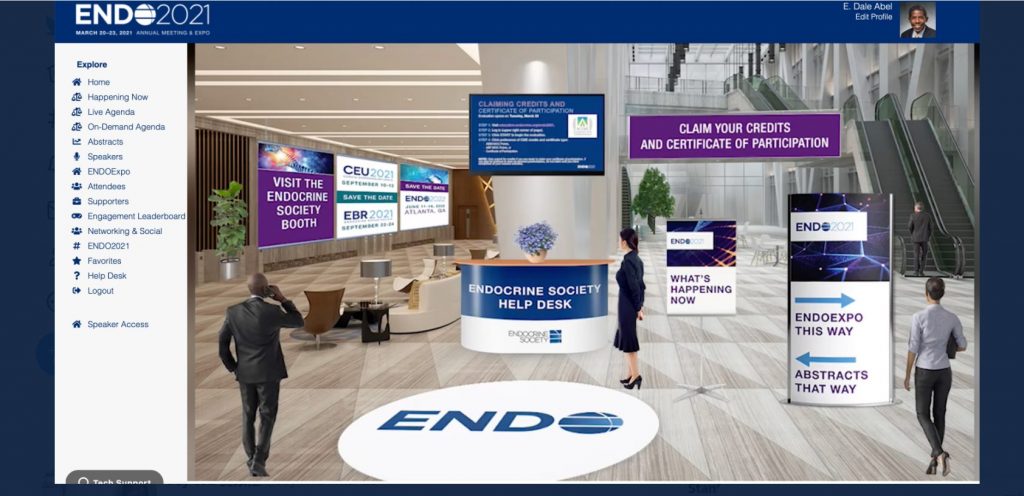
After the successes of the all-new ENDO Online 2020 and virtual versions of the Endocrine Society’s Clinical Endocrinology Update and Endocrine Board Review programs last year, even more records were broken in March with the first-ever all virtual ENDO 2021.
This virtual meeting of the minds saw more than 7,000 attendees from around the world, with the brunt attending from within the U.S. (4,157), but there were quite a number of people tuning in from Canada (27), Mexico (152), Brazil (37), the United Kingdom (22), Australia (168), and 137 tuned in from Thailand! And while the majority of attendees were clinical practitioners (3,000+), there were almost 900 clinical researchers and almost 500 basic scientists tuning in, with clinical fellows in training (672), graduate students (238), residents (346), educators (200+), and others all checking out this one-of-a-kind content.
One of the reasons for this “highlights” article is that there was no way you could catch every single session that was offered; there were 219 live and on-demand sessions, 46 live and on-demand Meet the Professor sessions, 24 oral abstract sessions, 10 ancillary symposia, six live plenary sessions, and 1,976 posters! There were also 17 different product theaters that had an average of over 400 attendees each with more than 50 exhibitors receiving an average of 161 visitors for each booth!
Suffice to say, in those four days from March 20 to 23, there was a lot to take in and chief among the benefits of ENDO 2021 being all virtual was that everything was literally right at your fingertips. Attendees saw for themselves that endocrine science was once again at the forefront of creating a better understanding of COVID-19; myriad groups of scientists presented their topical research on the biggest endocrine challenges related to the pandemic.
Researchers examined the implications of COVID-19 infection for individuals with certain comorbidities, including obesity, hyperglycemia, adrenal insufficiency, and vitamin D deficiency. The studies highlighted here include:
- “Obesity Is Associated with Intensive Care Use and Duration of ICU Stay but Not Mortality Among 3246 Patients Hospitalized with COVID-19”
- “Sugar is Not Always Sweet: Exploring the Relationship Between Hyperglycemia and COVID-19 in a Predominantly African American Population”
- “Risk of Complications in Children with Adrenal Insufficiency and COVID-19”
- “Pre-admission Vitamin D Supplementation in Patients with Low 25[OH]D May Improve COVID-19 Outcomes”
In each of these areas, their research represents cutting edge science, given that the pandemic is still a relatively new occurrence, and they have not had the time or opportunity to conduct long-term studies. What little is known about how COVID-19 affects or is affected by concomitant disease is thanks to resourcefulness and enterprise.
Obesity and COVID-19
Yu Mi Kang, MD, PhD, of Yale New Haven Health in New Haven, Conn., presented her team’s study on COVID-19 and obesity. With obesity being so widespread, and preliminary studies suggesting that it increases vulnerability to SARS-CoV-2 infection, Kang and team set out to elucidate the mechanisms by which obesity increases this susceptibility to infection or predisposes to worse COVID-19 outcomes. Given the currency of the COVID-19 pandemic, early studies on the subject were, by necessity, on the small side with short-term follow-up periods, among other design weaknesses that led to questions about the accuracy of results, particularly in terms of the relationship between body mass index (BMI), COVID-19 infection, and associated mortality. This team wanted to set the record straight.
“We aimed to determine the association of obesity with outcomes among patients hospitalized for COVID-19 using a large cohort with calculated BMI,” Kang says. The Yale Department of Medicine COVID Explorer (DOM-CovX) database contains clinical information across five hospitals in the Yale health system across Connecticut and Rhode Island. Using DOM-CovX, the team included 3,246 patients aged 18 years and older, who were hospitalized between March and September 2020 and had positive polymerase chain reaction (PCR) tests confirmed between 14 days prior to admission until the date of discharge.
“The primary endpoints were in hospital death or transition to hospice care, ICU admission, and the length of ICU stay,” Kang says. “We used the first weight on admission or the most recent weight within 90 days of admission, followed by manual chart review.” They used the World Health Organization (WHO) classifications of obesity: Grade 1 overweight = BMI of 25–29.9 kg/m, Grade 2 overweight = BMI of 30–39.9 kg/m, and Grade 3 overweight = BMI ≥40 kg/m.
Of the proportion of people hospitalized with COVID-19, less than 25% had normal weight, whereas 43% fell into the obesity category. The median age of all hospitalized patients with COVID-19 was 65; for those underweight, it was 78.5; for those with normal weight it was 75; for those overweight, it was 65; and for those with obesity, it was 59. Those with obesity were more likely to be female and more likely to have diabetes at baseline.
“[Our study] underscores the vulnerability of individuals with obesity during the current pandemic and emphasizes the need to ensure that obesity is given appropriate consideration in COVID-19 prevention and management.” – Yu Mi Kang, MD, PhD, Yale New Haven Health, New Haven, Conn.
“A total of 16.7% of our hospitalized COVID-19 patients died or transitioned to hospice care compared to the normal-weight group,” Kang says. In unadjusted analysis, the underweight group showed the highest crude mortality rates, and mortality across obesity class did not go up. Other findings included that about 25% of hospitalized patients were admitted to the ICU, and the obesity group showed a significantly higher crude ICU admission rate compared with the normal weight group. They also looked at ICU admission rate by obesity grade, and found, not surprisingly, that grade 3 obesity conferred the highest risk.
When they adjusted each analysis for age, gender, race, ethnicity, diabetes, chronic kidney disease, cardiovascular disease, neurological disease, liver disease, hypertension, immunosuppressive therapy, and respiratory disease, overall obesity as well as grades 2 and 3, again, not surprisingly, was associated with increased ICU admission compared to normal-weight individuals. Individuals with obesity also had a longer duration of ICU stay by almost 3 days compared with normal-weight individuals, who stayed an average of 6.6 days. Breaking the obesity group down by grade showed the expected incremental trend with individuals with grade 3 obesity staying in the ICU 10.2 days on average.
The surprise came when their adjusted results showed no significant association of obesity with in-hospital death or transition to hospice care, despite the higher likelihood of ICU admission and longer stays. Although the team has not definitively uncovered where this possible protective effect might come from, Kang posited that COVID-19-targeted therapies like dexamethasone and remdesivir use had become the protocol in patients with obesity, and this might have mitigated some of the effects attributable to obesity. Whether such an influence exists will of course require additional investigation.
Concluded Kang: “[Our study] underscores the vulnerability of individuals with obesity during the current pandemic and emphasizes the need to ensure that obesity is given appropriate consideration in COVID-19 prevention and management.” She furthermore suggests that having a reliable risk-stratification method that could be further applied to vaccination guidelines and COVID-19 management protocols is one way to achieve that important clinical goal.
Hyperglycemia and COVID-19
The relationship between hyperglycemia and COVID-19 in a predominantly African American population was discussed by Samara Skwiersky, MD, MPH, a second-year internal medicine resident physician at the State University of New York (SUNY) Downstate Medical Center in Brooklyn, N.Y.
At the time of her presentation, the pandemic was responsible for over 28 million cases of COVID-19 in the U.S. and more than 500,000 deaths. In New York City (as elsewhere), the more than 700,000 cases disproportionately affected African Americans, who are two to three times more likely than White American to die from COVID-19 infection. In New York City, Blacks have 300 deaths per 100,000 compared to 178 deaths per 100,000 in non-Hispanic Whites. The concomitant high prevalence of diabetes among Blacks got Skwiersky and team wondering how a prior diagnosis of diabetes could affect outcomes in patients with COVID-19. Although a few studies conducted during the pandemic have identified both diabetes and hyperglycemia independently as risk factors for worse clinical outcomes with COVID-19, no studies had focused on this relationship in African Americans. Swiersky and team filled that gap with their retrospective cohort study of all COVID-positive patients admitted to SUNY Downstate Medical Center, designated as a COVID-only center by New York Governor Andrew Cuomo, between March 1 and May 15, 2020. They collected patient demographics, clinical characteristics, and outcomes from the hospital’s electronic medical records system and used multivariate logistic regression analysis to calculate adjusted odds ratios for outcomes of mortality, intubation, ICU admission, and acute kidney injury (AKI) based on prior diagnosis of diabetes and admission blood glucose levels. They also performed a multiple linear regression analysis for the continuous outcome of length of stay.
“We found that patients without diabetes presenting with glucose >180 had fourfold increased odds of death, whereas those with a history of diabetes and glucose >180 had only 1.8 increased odds of death. These findings are consistent with other studies published prior to the pandemic, which found a greater association between hyperglycemia and mortality in patients hospitalized without a prior diagnosis of diabetes.” – Samara Skwiersky, MD, MPH, second-year internal medicine resident physician, State University of New York Downstate Medical Center, Brooklyn, N.Y.
Of the 982 patients hospitalized during the study time period, the 708 patients who tested positive for COVID-19, were at least age 18 years, and had sufficient data available for analysis were included in the final study cohort. This cohort was divided into subjects with and without diabetes and then again by admission blood glucose >140 or <140 and >180 or <180 mg/dL, based on the current American Diabetes Association guidelines recommending a target glucose of 140–180 for most patients during hospitalization. Of the cohort, 89% were Black, the mean age was 68 years, and 54% (383 patients) had a known history of diabetes.
Overall clinical outcomes included a sobering 40% crude mortality rate. When odds ratios were adjusted for age; sex; BMI; white blood cell count; creatinine; and history of hypertension, cardiovascular disease, and chronic kidney disease, overall, hyperglycemia on admission resulted in worse clinical outcomes in patients hospitalized with COVID-19 with and without diabetes. “Patients with diabetes who had an admission glucose >140 compared to those with glucose <140 had a significantly increased risk of intubation and ICU admission, whereas those with an admission glucose >180 had increased risk of mortality alone,” Swiersky says. In comparison, patients without diabetes with an admission glucose >140 had increased risk of mortality, ICU admission, intubation and AKI, whereas those with glucose >180 had increased risk of mortality, ICU admission, and intubation. The relationship between admission glucose of 140–180 and mortality in patients with and without diabetes was not statistically significant.
Thus, admission glucose levels outside of recommended levels is associated with inpatient mortality in patients with COVID-19 infection. “Specifically, we found that patients without diabetes presenting with glucose >180 had fourfold increased odds of death, whereas those with a history of diabetes and glucose >180 had only 1.8 increased odds of death,” Swiersky says. “These findings are consistent with other studies published prior to the pandemic, which found a greater association between hyperglycemia and mortality in patients hospitalized without a prior diagnosis of diabetes.”
Two big questions remain. One is whether hyperglycemia is the result of or a cause of more severe COVID-19 illness. Could intensive glucose control with more frequent monitoring and treatment with insulin to a target glucose of <140 improve outcomes in patients hospitalized with COVID-19? Current Endocrine Society guidelines recommend that all patients hospitalized with blood glucose >140 be monitored and treated with appropriate therapies, so it seems reasonable that patients with COVID-19 who present with hyperglycemia would require this much and more.
The second question is why patients without a history of diabetes fared worse than patients with diabetes despite similar blood glucose levels. Metformin taken by many patients with diabetes could be exerting a protective effect, but this hypothesis has not been studied. Swiersky also points out that a limitation of her team’s study is that hemoglobin A1c was not measured on admission, so distinguishing patients with undiagnosed diabetes from those with stress hyperglycemia caused by illness was not done.
Adrenal Insufficiency and COVID-19
Manish Raisingani, MD, of the University of Arkansas for Medical Sciences and Arkansas Children’s Hospital in Little Rock, Ark., presented research about the risk of complications in children with adrenal insufficiency and COVID-19, an area with scant existing data. Because of their lack of cortisol, children with adrenal insufficiency are unable to mount a normal stress response to infections, which can put them at a higher risk of complications from infections and means they are often given stress-dose steroids during infection.
Using the TriNet X database that collects information from healthcare organizations in 31 different countries, Raisingani and team compared children ages 0 to 18 years diagnosed with COVID-19 with and without adrenal insufficiency for complications including mortality, sepsis, and intubation. Among more than 600,000 children without adrenal insufficiency diagnosed with COVID-19 infection, 215 died, representing a relatively low risk of mortality of 0.03%. “The kids who had the diagnosis of adrenal insufficiency at least a month prior to the COVID-19 infection, had a much higher risk of mortality,” Raisingani says. “Their relative risk was almost 23 times higher.”
“It is very important for children with adrenal insufficiency to take precautions during these times — to take their medications properly as well as take their stress doses properly. Parents should also be reeducated about using the emergency injection of hydrocortisone as needed at home.” – Manish Raisingani, MD, University of Arkansas for Medical Sciences and Arkansas Children’s Hospital, Little Rock, Ark.
Knowing that children with adrenal insufficiency also tend to have respiratory illnesses, lupus, or secondary adrenal insufficiency from long-term steroid use, the team adjusted their findings, which brought the relative risk down to about fourfold higher. “So adrenal insufficiency can independently be associated with higher risk of mortality independent of other medical issues,” Raisingani says. With likelihood of sepsis and intubation, the adjusted risk was also higher in children with adrenal insufficiency compared to those without.
“It is very important for children with adrenal insufficiency to take precautions during these times — to take their medications properly as well as take their stress doses properly,” concludes Raisingani. Especially with schools having begun to reopen, stress dosing as soon as a child gets sick to prevent significant complications due to COVID-19 or any other infections is critical. “Parents should also be reeducated about using the emergency injection of hydrocortisone as needed at home.”
He also mentioned that distinguishing between primary and secondary adrenal insufficiency might change the data.
Vitamin D Deficiency and COVID-19
Sweta Chekuri, MD, and Sarah Baron, MD, MS, of Montefiore Health System and Albert Einstein College of Medicine in the Bronx, N.Y., presented research on how preadmission vitamin D supplementation in patients with low 25-hydroxy-vitamin D may improve COVID-19 outcomes. This team, knowing that vitamin D supplementation has demonstrated efficacy in respiratory illnesses like the flu and respiratory syncytial virus, wanted to know if repurposing this inexpensive treatment for COVID-19 infection might improve outcomes.
Their study population was all 124 adults with COVID-19 admitted to Montefiore Medical Center between March 11 and June 2, 2020 with a preadmission 25-hydroxy-vitamin D <30. They defined severe COVID-19 disease as mechanical ventilation or death, insufficient vitamin D level as 20–30, and vitamin D deficiency as <20. Of the predominantly female and predominantly Hispanic cohort, the median age was 64 years, and the median BMI was 29.1; 64 were not supplemented with vitamin D, and 60 were supplemented with ≥1000 units of cholecalciferol or ergocalciferol weekly.
“In our primary outcome, we noted vitamin D supplementation with ≥1000 units weekly had no significant effect on severe COVID-19 in the unadjusted or adjusted model,” Chekuri says. “But in subgroup analysis, we noted lower odds of severe COVID-19 outcomes in the unadjusted model for those patients deficient with 25-hydroxy-vitamin D, which also held true when supplementation was ≥5000 units weekly.” These findings, however, were not statistically significant.
In patients in the vitamin D-deficient group, 39.1% of those not supplemented had severe COVID-19 outcomes, but only 25% of those supplemented with ≥1000 units weekly had severe COVID-19 outcomes, and only 21.7% of those supplemented with ≥5000 units weekly (again, not statistically significant).
“In our primary outcome, we noted vitamin D supplementation with ≥1000 units weekly had no significant effect on severe COVID-19 in the unadjusted or adjusted model. But in subgroup analysis, we noted lower odds of severe COVID-19 outcomes in the unadjusted model for those patients deficient with 25-hydroxy-vitamin D, which also held true when supplementation was ≥5000 units weekly.” – Sweta Chekuri, MD, Montefiore Health System and Albert Einstein College of Medicine, Bronx, N.Y.
“Though it was not significant, our data demonstrated a difference in severe COVID-19 outcomes based on vitamin D supplementation,” Chekuri says. “This effect was more pronounced in patients with preadmission 25-hydroxy-vitamin D <20.” As only half of the patients in their study with a level that low were supplemented, Chekuri and Baron and team suggest that providers should proactively prescribe vitamin D supplementation to any patient at risk for COVID-19 with deficient vitamin D levels to offer protection against worse outcomes. This begs the question, should everyone go have their levels checked? Probably not everyone, explains Baron, but if you are symptomatic, or you are at risk for COVID-19, see your provider and get it checked. “If it’s low, supplement.”
As more and more people get vaccinated each day, hopes are high that ENDO 2022 will see throngs of endocrinologists from around the world converge in Atlanta, Ga., next June. For those who can’t make the trip, no doubt there will be a virtual option available. However, whether in person or via an electronic device, breakthroughs in endocrine science will continue to improve the health of millions around the world.
Horvath is a freelancer writer based in Baltimore, Md. She wrote about health disparities in various minority groups in the May issue.
Log On for More ENDO 2021 Highlights
ENDO 2021 was jam packed so you might have missed out on a few things. Be sure to check out the highlights online where you can see:
- ENDO Faculty Interviews
- Expert Overviews
- Oral Session Summaries
- Poster Podcasts
- ENDO Leadership Interviews
And be sure to tune into the interview with incoming Endocrine Society president Carol Wysham, MD, who talks about her objectives for the next year as well as her personal highlights from ENDO 2021.

