Introducing a Comprehensive Blueprint to Address the Diabetes Complication of Hypoglycemia.
The Endocrine Society leads effort to reduce the incidence of hypoglycemia by developing a comprehensive blueprint with diabetes stakeholders recommending actions for how the community can effect change.
Download a complete version of the Blueprint, including references.
The numbers are increasing and are alarming: more than 29 million Americans are living with diabetes and an additional 86 million are at risk for developing the disease. The impact to the healthcare system is vast. The Economic Costs of Diabetes in the U.S. in 2012 estimated that diabetes costs $245 billion, including $176 billion in direct medical costs and $69 billion in reduced productivity. Consequently, the Endocrine Society has prioritized the need to prevent diabetes and effectively manage its complications.
In order to achieve this goal, the Society is well aware that it must work with other diabetes stakeholders to design, implement, and evaluate initiatives that will improve the prevention and management of diabetes, thereby reducing the burden associated with complications such as hypoglycemia. In 2015 the Endocrine Society conducted a roundtable and brought together stakeholders from federal agencies, patient and provider groups, payers, and industry to discuss how the diabetes community can work together to affect change.
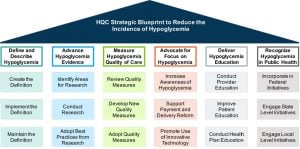
The Roundtable participants agreed that addressing the burden of hypoglycemia is critical and focused efforts on working together to determine actions needed to increase national awareness and execute tactics that improve its prevention and management in the U.S. To facilitate this need, the Endocrine Society created a working group known as the Hypoglycemia Quality Collaborative (HQC) to develop a blueprint (Blueprint) that provides a comprehensive approach to reducing the incidence of hypoglycemia and ensuring that patients and providers receive the tools they need to prevent and manage the complication. The resulting Blueprint contains the following six domains that together create a comprehensive framework for addressing hypoglycemia:
- Defining and describing hypoglycemia to support standards of care
- Advancing hypoglycemia evidence to reduce gaps in care
- Measuring and improving the quality of care for patients who experience hypoglycemia
- Advocating for an increased focus on hypoglycemia
- Delivering hypoglycemia prevention and management education
- Recognizing hypoglycemia as a public health issueEach of these key domains include three strategic areas which contain specific recommendations for how diabetes stakeholders can contribute to preventing and managing hypoglycemia. Below is a summary of the Blueprint and its recommendations:
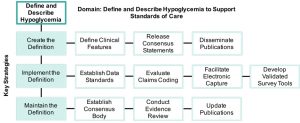
Defining and Describing Hypoglycemia to Support Standards of Care
The current definition of hypoglycemia does not support differentiation of hypoglycemic episodes by severity. The foundation for improving the prevention and management of hypoglycemia is an updated definition that accounts for differing hypoglycemia severity. A comprehensive and standardized definition can then be adopted in research, clinical guidance and decision support tools, and reimbursement models that reward quality.
Create a New Definition: A new definition of hypoglycemia must be created through a review of evidence and include both clinical values and descriptions of positive and negative symptoms. The definition should have consensus support and facilitate the recognition, tracking, and treatment of different hypoglycemia severity (Note: JDRF is currently leading efforts to develop a consensus definition for differing hypoglycemia severity).
- HQC Recommendation: A new definition should include both a symptom-complex and a biochemical definition since there are many factors that may affect whether a patient has symptoms.
- HQC Recommendation: To support prevention and management, a new definition should allow for capture of data related to pre- and post-hypoglycemia events in acute, post-acute, and community care settings (e.g., outpatient or home), including patient factors such as fears and beliefs of hypoglycemia.
Implement the Definition: The new definition will require a technical expert panel to establish data standards and a set of standardized data elements for consistent electronic capture and transfer of hypoglycemia data by severity. Similarly, diagnostic and procedural coding (e.g., ICD, CPT) must be evaluated to support comprehensive capture of hypoglycemic episodes by severity. These steps provide the foundation for development of survey-based tools and testing of new hypoglycemia quality measures.
- HQC Recommendation: To accelerate the adoption of a new definition, large commercial payers and provider organizations should be engaged to adopt the consensus definition and disseminate it to members within their organizational network such as through the organization’s diabetes standards of care.
Maintain the Definition: The definition of hypoglycemia will require a consensus body that periodically monitors and conducts targeted literature reviews to update the evidence base and support definition maintenance.
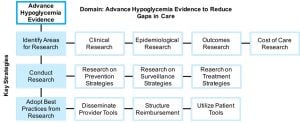
Advancing Hypoglycemia Evidence to Reduce Gaps in Care
Current research related to glycemic control often focuses on the prevention and management of hyperglycemia. The federal government must increase funding for research at the National Institutes of Health (NIH) and the Centers for Disease Control and Prevention (CDC) to reduce gaps in evidence related to hypoglycemia prevention and management. This research should elucidate the short-term and long-term effects of hypoglycemia on patient outcomes so that standards of care can be updated or newly developed.
Identify Areas for Research: Major gaps in hypoglycemia evidence should be identified so that research may be conducted to design prevention and management strategies that reduce gaps in care for hypoglycemia.
- HQC Recommendation: Major gaps in evidence include:
- The pre-cursor clinical indicators of severe hypoglycemia such as frequent or protracted non-severe hypoglycemia;
- The incidence of hypoglycemia by severity level including events in emergency and outpatient settings;
- The short-term effects of hypoglycemia on outcomes (e.g., arrhythmias, cardiovascular events, and cerebrovascular events);
- The long-term effects of hypoglycemia (e.g., quality of life, functional status);
- The patient characteristics that increase hypoglycemia risk such as age, ethnicity, beliefs and fears of hypoglycemia, DSME status, and therapy choices (e.g., insulin, sulfonylurea, analog insulin, or bolus insulin);
- The indirect costs of hypoglycemia (e.g., lost productivity/absenteeism);
- The best practices for using continuous glucose monitor (CGM) data to inform appropriate medication or lifestyle modifications;
- The best practices for standardized reporting of CGM data.
Conduct Research: Research that is conducted should have the objective of informing prevention, surveillance, and management approaches that account for differing hypoglycemia severity.
- HQC Recommendation: Research on patient beliefs and attitudes impacting behavior is a high priority in order to improve prevention and management strategies, especially for patients at risk for recurrent severe hypoglycemia.
- HQC Recommendation: Research to improve surveillance should focus on elucidating the incidence of hypoglycemia by severity and across settings of care such as the utilization of emergency medical and outpatient services related to hypoglycemia.
The federal government must increase funding for research at the National Institutes of Health (NIH) and the Centers for Disease Control and Prevention (CDC) to reduce gaps in evidence related to hypoglycemia prevention and management.
Adopt Best Practices from Research: Action by all stakeholders is needed for comprehensive adoption of best practices from research. Medical specialty societies must make timely updates to clinical guidance documents and educational materials; primary care teams must incorporate new surveillance strategies; diabetes educators and patient advocates must update educational materials; commercial and public payers must review and adjust reimbursement and benefit designs; and health information technology vendors and digital health manufacturers must provide tools that support new standards of care.
- HQC Recommendation: To encourage adoption of new best practices for prevention and management of hypoglycemia based on severity, medical specialty societies should develop a communication strategy with key messaging for engagement with regulators and payers.
- HQC Recommendation: Medical specialty societies should engage with primary care providers to identify opportunities to support primary care providers in adopting best practices for hypoglycemia prevention and management.
- HQC Recommendation: Payers and providers should actively consider ways to incorporate CGM data into clinical decision making for prevention and management of hypoglycemia in high risk individuals.
Measuring and Improving Hypoglycemia Quality of Care
Quality measures for diabetes that specifically assess prevention and management of hypoglycemia are lacking. Evidence-based quality measures are needed that support coordinated, timely, and safe prevention and management of hypoglycemia. Diabetes stakeholders must coordinate to develop and test hypoglycemia quality measures to support improved hypoglycemia outcomes.
Review Current Quality Measures: Current claims, electronic, and patient-reported outcomes measures for diabetes should be reviewed and updated, if necessary, to improve alignment of the measures with current clinical guidance for preventing and managing severe hypoglycemia.
- HQC Recommendation: Current measures should be reviewed and updated to promote the use of individualized HbA1c target goals and SMBG targets (e.g., fasting, pre-meal, post prandial and bedtime blood glucose), distinguish differing hypoglycemia severity, and evaluate whether DSME was received/completed.
Develop New Quality Measures: New quality measures are needed that support surveillance of individuals at risk for hypoglycemia across settings of care, use of shared decision-making for medication selection, and evaluation of patient attitudes, fears, and behaviors related to blood glucose management.
- HQC Recommendation: Structural measures should be developed to support timely communication to notify a patient’s primary care provider of a hypoglycemia-related emergency room visit or a medication switch following an inpatient admission.
- HQC Recommendation: Process measures should be developed to improve outpatient hypoglycemia risk evaluation, including less severe hypoglycemia, and use of individualized HbA1c targets goals.
- HQC Recommendation: Patient-reported outcomes measures are needed to evaluate fears of hypoglycemia, effect on quality of life, loss of productivity, and confidence with self-management.
- HQC Recommendation: Outcome measures that use clinical endpoints other than HbA1c are needed to better understand glycemic control. New measures could use multiple metrics including HbA1c, time-in-range, and hypoglycemia as potential endpoints for evaluating glycemic control.
Adopt Current and New Quality Measures: Evidence-based measures that are closely tied to outcomes and patient-centered interests must be adopted in national quality improvement, provider accreditation, and public reporting programs.
- HQC Recommendation: Physician Consortium for Practice Improvement (PCPI) measures for DSME[i] should be submitted for adoption in Centers for Medicare & Medicaid Services (CMS) inpatient and outpatient quality improvement programs as well as for use by commercial payers.
- These measures can be submitted to CMS for adoption in the Physician Quality Reporting System (PQRS) or future Merit-Based Incentive Payment System (MIPS) using mechanisms such as the Qualified Clinical Data Registry (QCDR) reporting option.
- HQC Recommendation: Quality measures such as NQF 2363: Glycemic Control should be submitted for adoption in the National Committee for Quality Assurance’s (NCQA) Diabetes Recognition Program and The Joint Commission (TJC) disease specific certification programs.
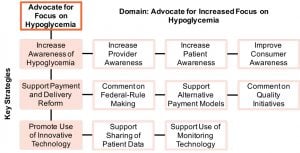
Advocating for Increased Focus on Hypoglycemia
Advocacy is an effective tool to increase national focus on hypoglycemia. Through advocacy, diabetes stakeholders become more aware of the need to devote resources and attention towards preventing and managing hypoglycemia.
Increase Awareness of Hypoglycemia: Advocacy through the development of policy positions, educational events, and engagement with other diabetes stakeholders should improve awareness of the harm of hypoglycemia, describe methods for prevention and management, and promote increased funding of research that supports provider and patient clinical decision-making for hypoglycemia.
- HQC Recommendation: Patients/caregivers should be engaged by diabetes educators, patient advocacy groups, and social workers regarding self-management techniques as well as protective rights in the workplace.
- HQC Recommendation: Primary care providers/organizations and advanced practice providers should be engaged to expand their role in both diabetes management and hypoglycemia prevention by referring patients to certified diabetes educators or patient education programs that are typically covered services.
- HQC Recommendation: Providers should be engaged regarding the impact of hypoglycemia relative to hyperglycemia and the importance of managing hypoglycemia by setting appropriate HbA1c and SMBG targets, using appropriate medications, educating on diet and exercise, and providing blood glucose monitoring education and tools.
- HQC Recommendation: Members of medical specialty societies should be engaged regarding the importance of legislative mechanisms for improving diabetes care such the Diabetes Clinical Care Commission Act.
Support Payment and Delivery Reform: Care models that incentivize coordinated, timely, safe, and accessible care for diabetes should be promoted through engagement with state health officials, federal rule-making, and outreach to commercial payers.
- HQC Recommendation: States with Diabetes Action Plans (Kentucky, Texas Illinois, Louisiana, New Jersey, North Carolina, North Dakota, Oregon, and Washington) should be engaged to include explicit tactics for preventing and managing hypoglycemia.
- States without Diabetes Action Plans should be encouraged to develop action plans that specifically include tactics for preventing and managing hypoglycemia.
- HQC Recommendation: Public and commercial payers should be engaged regarding the value of reimbursement strategies that promote evidence-based care for hypoglycemia.
- HQC Recommendation: Policy makers should be engaged regarding the value of reimbursement that promotes evidence-based prevention and management for hypoglycemia to reduce the significant costs and poor outcomes of hypoglycemia.
Promote Use of Innovative Technology: Advocacy to federal regulators, commercial payers, and providers should promote patient access to glucose monitoring tools (e.g., CGMs, strip meters) and education to support providers to utilize data from these tools to inform prevention and management decisions.
- HQC Recommendation: Public and commercial payers should be engaged regarding the importance of digital health and remote monitoring technologies for evaluating the burden of hypoglycemia, improving provider care coordination, and promoting shared decision-making.
- HQC Recommendation: Public and commercial payers should be engaged to promote access and use of active surveillance tools such as CGMs for patients at high risk for severe hypoglycemia.
- HQC Recommendation: Electronic medical record vendors should be engaged to integrate clinical decision support tools that allow for capture and transfer of hypoglycemia data by severity.
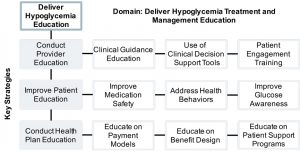
Delivering Hypoglycemia Prevention and Management Education
Stakeholder education is a significant activity that is necessary to increase the use of evidence-based standards of care for prevention and management of hypoglycemia. Such education is important across settings of care and especially for patients and providers directly involved in the delivery of care.
Conduct Provider Education: All primary care healthcare professionals should receive hypoglycemia prevention and management education regardless of care setting. Hypoglycemia-specific education is needed to increase the use of individualized HbA1c and SMBG targets, referral of patients to DSME programs/diabetes educators, shared decision-making for management goals such as medication selections, discussion of barriers to medication adherence such as patient fears, and appropriate use of technology to prevent and manage hypoglycemia.
- HQC Recommendation: Initiatives to educate on new prevention and management approaches for hypoglycemia must be updated to include recommendations by hypoglycemia severity. These initiatives should also consider modifications to the provider’s workflow.
- HQC Recommendation: Providers should receive education regarding the interpretation and use of CGM and SMBG tools, including use and definition of multiple basal rates.
Improve Patient Education: Patient education is vital for improving outcomes, however, referral rates to educational programs are too low[i]. Patients should be referred to an accredited or recognized diabetes education program with the overall objective to support self-care behaviors, problem solving, and shared decision-making with the healthcare team.
- HQC Recommendation: Patient education initiatives should meet the National Standards for Diabetes Self-Management Education and Support.
- HQC Recommendation: Hypoglycemia-specific education should be targeted by age and gender, sensitive to the number of hours a patient has available, and ideally include training from behaviorists, nurses, dietitians, and exercise physiologists.
- HQC Recommendation: Hypoglycemia-specific training should include education on glucose pattern recognition and self-management actions, medication safety, fears of hypoglycemia, hypoglycemia unawareness, nutrition and lifestyle strategies, and strategies for appropriate glucose monitoring.
- HQC Recommendation: The use of telephonic/mobile patient education should be expanded with digital education targeted to those who will benefit most.
- HQC Recommendation: Patient-centered perspectives that encompass the experience of hypoglycemia, impact on quality of life, and strategies for self-management should be provided to patients.
Conduct Health Plan Education: Health plans have the ability directly influence provider and patient behavior based on reimbursement and benefit design. Education of both regional and national health plans on reimbursement and benefit design that improves hypoglycemia prevention and management is needed.
- HQC Recommendation: Regional payers and payers should be educated on the importance of reimbursement and benefit design that includes case management for individuals with diabetes from nurses or dietitians as mechanisms to reduce the frequency, impact, and incidence of severe hypoglycemia.
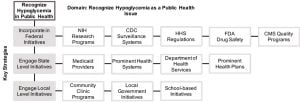
Recognizing Hypoglycemia as a Public Health Issue
Many diabetes public health programs currently exist at federal, state, and local levels. Within these programs, the topic of hypoglycemia must become a point of emphasis. By elevating the topic of hypoglycemia as a public health issue, diabetes stakeholders have a mechanism to significantly improve national awareness of hypoglycemia and reduce its incidence for any severity.
Incorporate in Federal Initiatives: Federal agencies must ensure that hypoglycemia is consistently reflected in research programs, surveillance systems, regulation, drug safety, and quality programs.
- HQC Recommendation: Diabetes stakeholders should engage with the agencies of the Department of Health and Human Services (HHS) to promote focus on hypoglycemia in federal programs and regulations.
- HQC Recommendation: The NIH should increase funding for research to improve prevention and management of hypoglycemia.
- HQC Recommendation: The programs of the CDC should support national hypoglycemia surveillance.
- HQC Recommendation: Important topics such as hypoglycemia in a public health context should be submitted to the Diabetes Mellitus Interagency Coordinating Committee, a workgroup of federal agencies that coordinates government components to work together to address issues in diabetes.
Engage State Level Initiatives: Medicaid providers and state-level Departments of Health and Human Services (DHHS) should incorporate hypoglycemia awareness and risk reduction into public health initiatives.
- HQC Recommendation: To affect change at the state level, important topics in diabetes such as hypoglycemia awareness and risk reduction should be reflected in state-level Diabetes Action Plan legislation.[i]
- HQC Recommendation: State-level initiatives should be delivered in a culturally sensitive format based upon the state’s diabetes population and educate on the use of technology, health literacy, and numeracy.
- HQC Recommendation: State-level DHHS should coordinate with prominent health systems and health plans in the high-priority regions of the state.
Engage Local Level Initiatives: In collaboration with state agencies, local entities can promote hypoglycemia public health awareness and distribute educational resources through clinics, local government, and schools.
- HQC Recommendation: To effectively deliver information and educate communities on pediatric diabetes hypoglycemia prevention and management, programs should be developed in collaboration with school nursing organizations such as National Association of School Nurses.
- HQC Recommendation: Diabetes and hypoglycemia public health resources should be culturally and linguistically appropriate to successfully engage an ethnically diverse diabetes patient population.
- HQC Recommendation: Community and socio-ethnic factors that contribute to hypoglycemia should be identified and targeted strategies must be used to prevent and manage hypoglycemia at a local level.
Moving Forward
The Blueprint has laid out opportunities that can affect change in six domains, offering specific strategies to reduce the incidence of hypoglycemia. It is the hope of the HQC that this Blueprint will elevate the issue of hypoglycemia to national importance, and provide opportunities for stakeholders to work together to improve the prevention and management of hypoglycemia.
The Hypoglycemia Quality Collaborative Blueprint is an initiative spearheaded by the Endocrine Society in conjunction with: Abbott Diabetes Care Inc., Aetna Inc., American Association of Clinical Endocrinologists, American Association of Diabetes Educators, American College of Physicians, American Diabetes Association, Astrazeneca LP, Close Concerns, Dexcom, Inc., Lilly USA, LLC, JDRF, Johnson & Johnson Joslin Diabetes Center, Medtronic Diabetes, Merck & Co., Inc., Novo Nordisk Inc., PQA Alliance, and T1D Exchange.
Endocrine Society would like to thank Merck & Co. for their generous support of the Hypoglycemia Quality Collaborative Blueprint.